ARTIFICIAL INTELLIGENCE IN EMERGENCY AND INTENSIVE CARE MEDICINE - BENEFIT OR RISK?
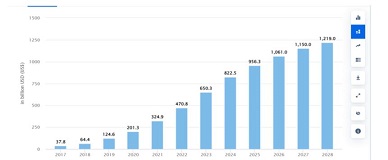
Downloads
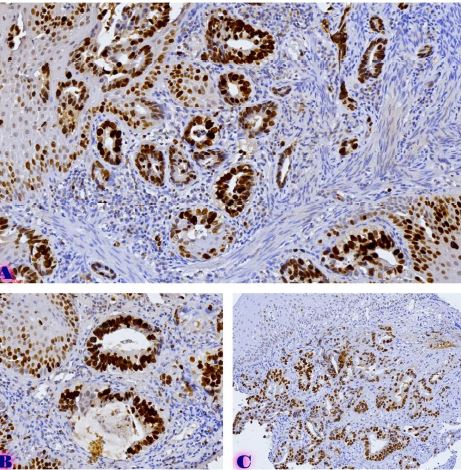
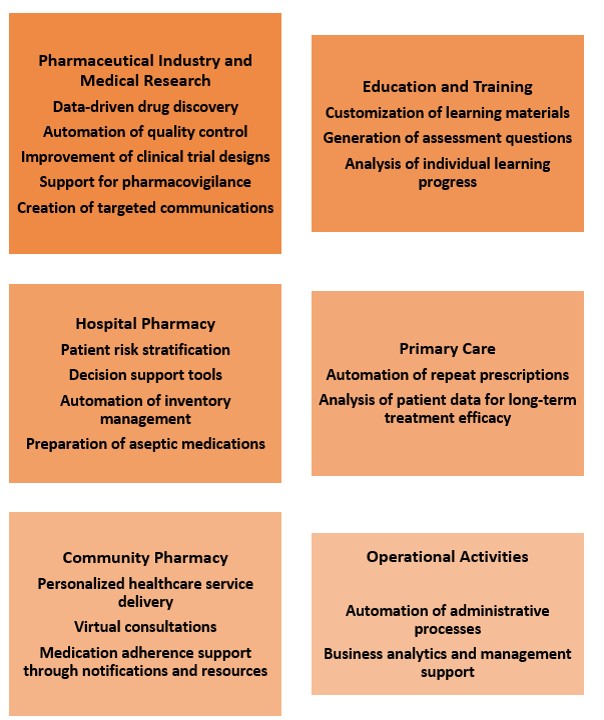
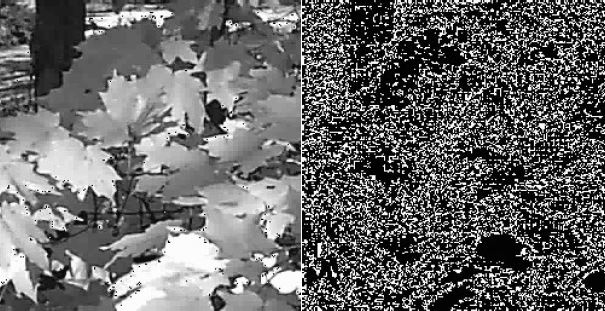
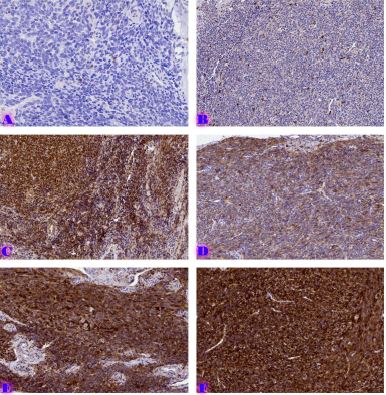
Artificial intelligence (AI) is transforming emergency and intensive care medicine by enabling earlier detection, faster diagnosis, and more precise decision-making in time-critical situations. AI-based systems are increasingly used to interpret chest X-rays, CT scans, ultrasound images, and ECGs for identifying pneumothorax, pneumonia, acute respiratory distress syndrome (ARDS), arrhythmias, and ischemia with remarkable accuracy.
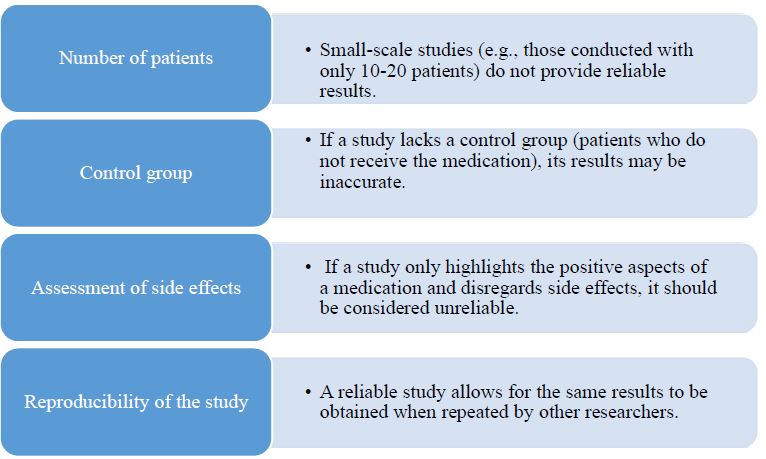
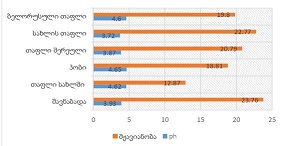
The U.S. Food and Drug Administration (FDA) has approved an AI-powered system that automatically detects pneumothorax with 100% sensitivity for large and 96% for small cases, and 94% specificity - substantially reducing false alarms. Such models help distinguish genuine emergencies from artifacts caused by motion, sensor errors, or benign physiological variations, improving workflow efficiency and clinical prioritization.
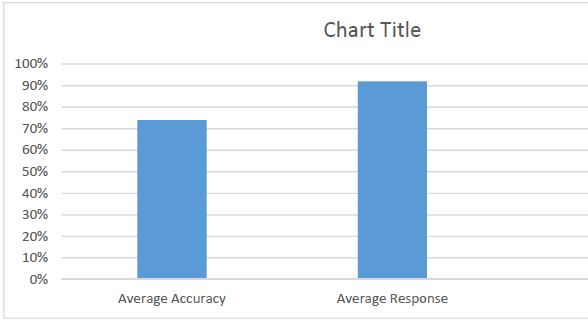
A key example of successful integration is the Targeted Real-time Early Warning System (TREWS), validated in a multicenter prospective study. TREWS enabled earlier identification and treatment of sepsis, reducing absolute mortality by approximately 4.5%. When clinicians responded to alerts within three hours, mortality decreased by 18% relative to baseline. The system demonstrated 82% sensitivity and was well accepted by clinicians (89%), highlighting its clinical reliability and usability.
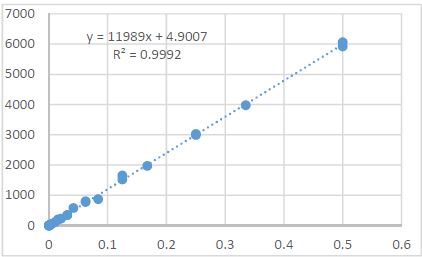
A PRISMA-guided meta-analysis of prospectively validated studies further confirmed the effectiveness of AI-based Early Warning Systems (EWS). Compared with traditional scores such as NEWS and APACHE II/III, which rely mainly on vital signs, AI models using neural networks, logistic regression, and random forest algorithms achieved superior predictive performance. Pooled results indicated significantly lower mortality (OR = 0.69, 95% CI 0.60–0.79) and shorter hospital stays ( - 0.35 days, p = 0.04). Rapid Response Team activations were also reduced, suggesting better early recognition of deterioration.
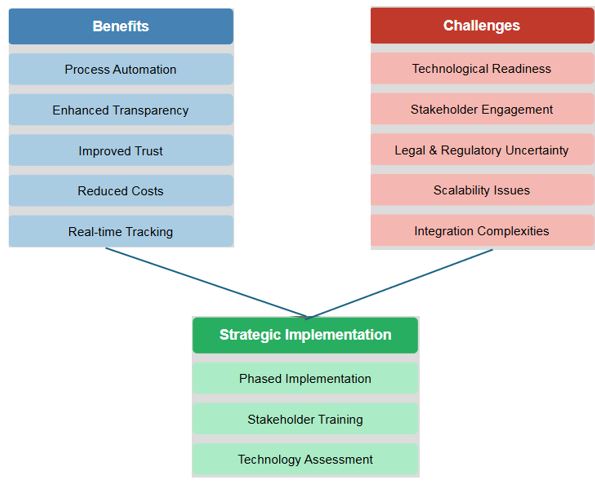
Despite these benefits, challenges persist. The limited interpretability of “black-box” models, need for clinician training, data quality concerns, and ethical considerations around fairness and access must be addressed to ensure safe implementation.
AI has proven its potential as a powerful ally in emergency and critical care - enhancing accuracy, efficiency, and patient outcomes - yet its responsible use requires transparency, collaboration, and continuous evaluation to maintain trust and safeguard patient safety.
Downloads
Copyright (c) 2025 Georgian Scientists

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.