Problemic issues in Molecular Characterization, Risk of Progression and Recurrence of Basal Cell and Squamous Cell Carcinomas of the Skin
Downloads
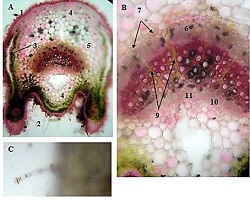
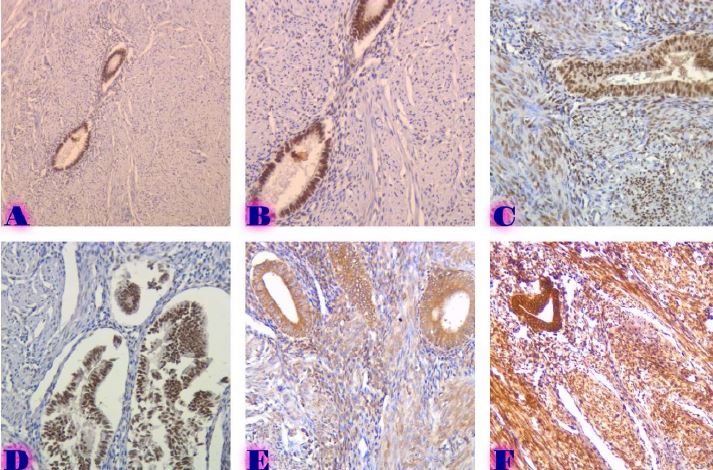
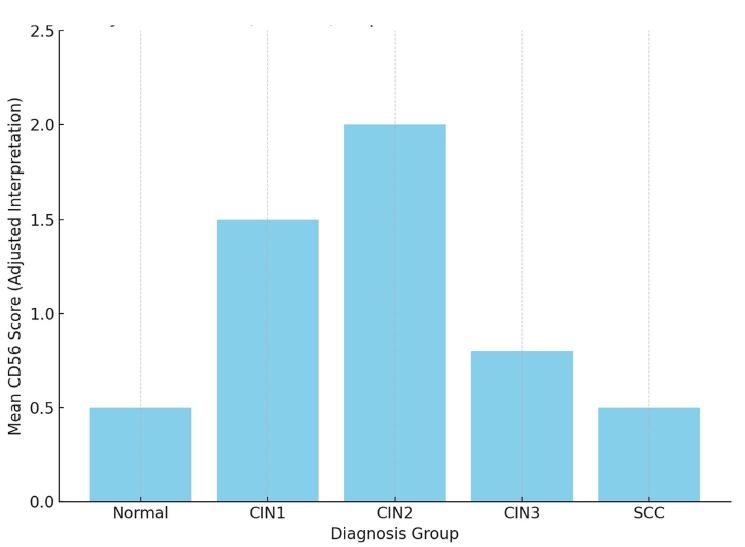
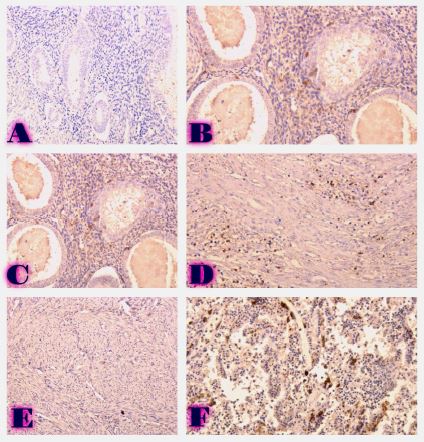
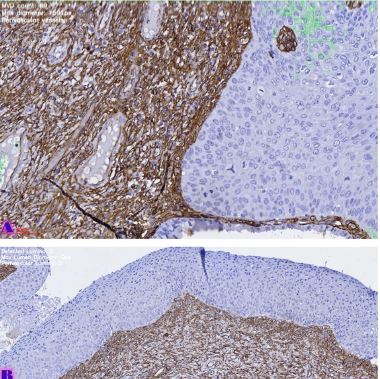
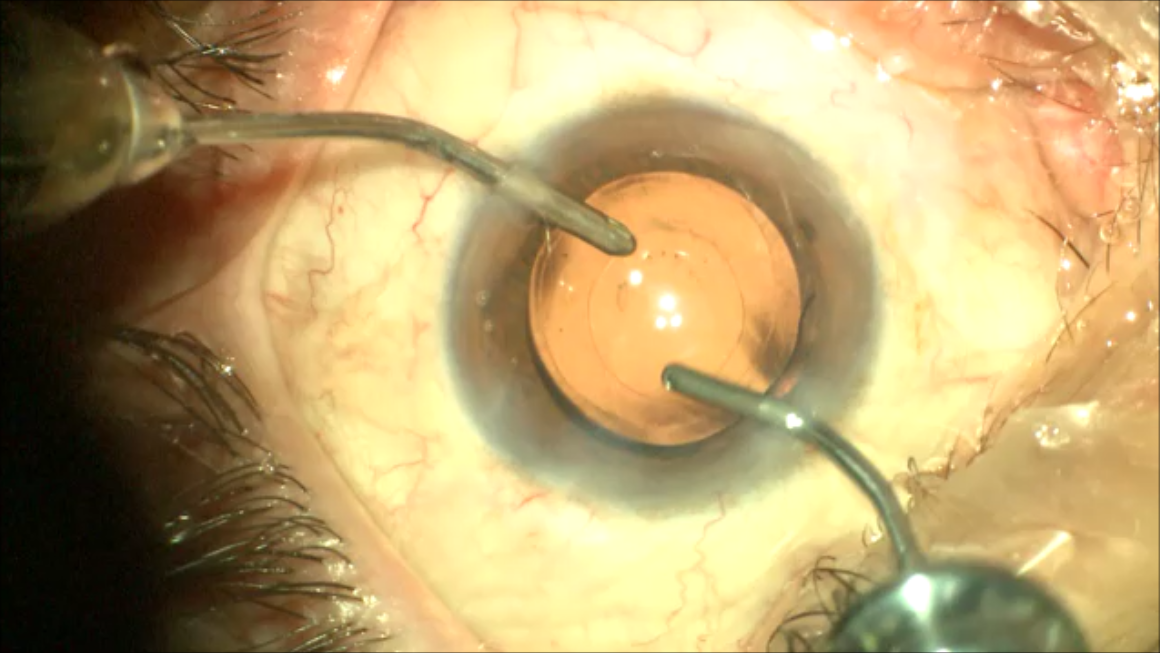
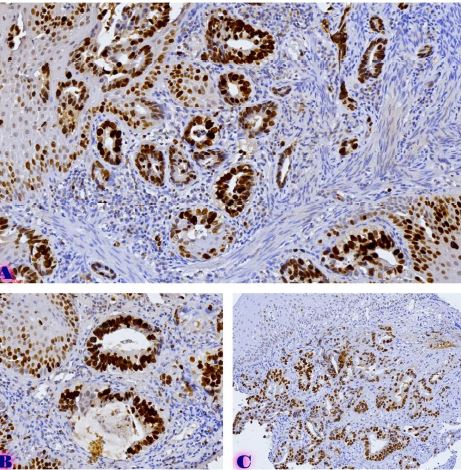
Non-melanoma skin tumors are a fairly common. Squamous cell carcinoma of the skin is characterized by particularly high malignancy, which is due to a high ability to metastasize. However, it has also been shown that patients with basal cell carcinoma of the skin have an increased risk of developing squamous cell carcinoma. The molecular phenotype of these tumors, as well as markers of progression, are not well studied. There is also no clear opinion about the origin of these tumors, although it is assumed that both of them have a common progenitor cell, namely, basal cells of the skin appendages of basal cell carcinoma, and basal cells of the epidermis of squamous cell carcinoma. In the current literature, there are only sparse and conflicting data on molecular markers of non-melanoma skin tumors and the risk of their progression. In addition, the correlation between dermoscopic data and histopathological characteristics of nonmelanocytic skin tumors has not been studied. The molecular characteristics of non-melanoma skin tumors, basal cell carcinoma and squamous cell carcinoma of the skin need to be studied in detail, in particular the risk markers of progression and recurrence of these tumors. Correlation between dermoscopic and histopathological data can also reveal valuable information. Therefore, it is important to study the phenotypic characteristics of basal cells and use their molecular characteristics to assess the risk of recurrence and progression of the mentioned diseases.
Downloads
R. L. Siegel, K. D. Miller, and A. Jemal, “Cancer statistics, 2020.,” CA Cancer J Clin, vol. 70, no. 1, pp. 7–30, 2020, doi: 10.3322/caac.21590.
D. Didona, G. Paolino, U. Bottoni, and C. Cantisani, “Non Melanoma Skin Cancer Pathogenesis Overview.,” Biomedicines, vol. 6, no. 1, Jan. 2018, doi: 10.3390/biomedicines6010006.
L. L. Griffin, A. Faisal, R. Ali, and J. T. Lear, “CMJv16n1-Griffin.indd,” 2016.
A. Combalia and C. Carrera, “Squamous Cell Carcinoma: An Update on Diagnosis and Treatment,” Dermatol Pract Concept, p. e2020066, Jun. 2020, doi: 10.5826/dpc.1003a66.
H. Rönsch and A. Bauer, “The Preventive Value of Sun Protection,” 2021, pp. 316–328. doi: 10.1159/000517641.
S. I. Goolamali, “Non-melanoma Skin Cancer in HIV Infection: the Role of Human Papillomavirus (HPV), Individual Immunogenotype (HLA ’tissue type’) and Merkel Cell Polyomavirus (MCV),” 2020.
M.-M. Chren, E. Linos, J. S. Torres, S. E. Stuart, R. Parvataneni, and W. J. Boscardin, “Tumor Recurrence 5 Years after Treatment of Cutaneous Basal Cell Carcinoma and Squamous Cell Carcinoma,” Journal of Investigative Dermatology, vol. 133, no. 5, pp. 1188–1196, May 2013, doi: 10.1038/jid.2012.403.
Q.-J. Wu et al., “Shift work and health outcomes: an umbrella review of systematic reviews and meta-analyses of epidemiological studies,” Journal of Clinical Sleep Medicine, vol. 18, no. 2, pp. 653–662, Feb. 2022, doi: 10.5664/jcsm.9642.
M. Wen, H. Ren, S. Zhang, T. Li, J. Zhang, and P. Ren, “CT45A1 promotes the metastasis of osteosarcoma cells in vitro and in vivo through β-catenin,” Cell Death Dis, vol. 12, no. 7, p. 650, Jul. 2021, doi: 10.1038/s41419-021-03935-x.
A. Dongre et al., “Direct and Indirect Regulators of Epithelial-Mesenchymal Transition-Mediated Immunosuppression in Breast Carcinomas.,” Cancer Discov, vol. 11, no. 5, pp. 1286–1305, 2021, doi: 10.1158/2159-8290.CD-20-0603.
B. Wang, X. Li, L. Liu, and M. Wang, “β-Catenin: oncogenic role and therapeutic target in cervical cancer.,” Biol Res, vol. 53, no. 1, p. 33, Aug. 2020, doi: 10.1186/s40659-020-00301-7.
S. Ramón y Cajal et al., “Clinical implications of intratumor heterogeneity: challenges and opportunities,” Journal of Molecular Medicine, vol. 98, no. 2. Springer, pp. 161–177, Feb. 01, 2020. doi: 10.1007/s00109-020-01874-2.
S. R. Georgescu et al., “Tumour Microenvironment in Skin Carcinogenesis,” 2020, pp. 123–142. doi: 10.1007/978-3-030-36214-0_10.
“Melanoma and nonmelanoma skin cancer.,” Curr Opin Oncol, vol. 3, no. 2, pp. 420–32, Apr. 1991, doi: 10.1097/00001622-199104000-00024.
M. L. Council, “Common Skin Cancers in Older Adults,” Clin Geriatr Med, vol. 29, no. 2, pp. 361–372, May 2013, doi: 10.1016/j.cger.2013.01.011.
V. Mittal, “Epithelial Mesenchymal Transition in Tumor Metastasis,” Annual Review of Pathology: Mechanisms of Disease, vol. 13, pp. 395–412, Jan. 2018, doi: 10.1146/ANNUREV-PATHOL-020117-043854.
K. T. Yeung and J. Yang, “Epithelial-mesenchymal transition in tumor metastasis,” Mol Oncol, vol. 11, no. 1, pp. 28–39, Jan. 2017, doi: 10.1002/1878-0261.12017.
S. Labiano, A. Palazon, and I. Melero, “Immune response regulation in the tumor microenvironment by hypoxia,” Semin Oncol, vol. 42, no. 3, pp. 378–386, Jun. 2015, doi: 10.1053/J.SEMINONCOL.2015.02.009.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.